In vitro fertilisation
In vitro fertilization process
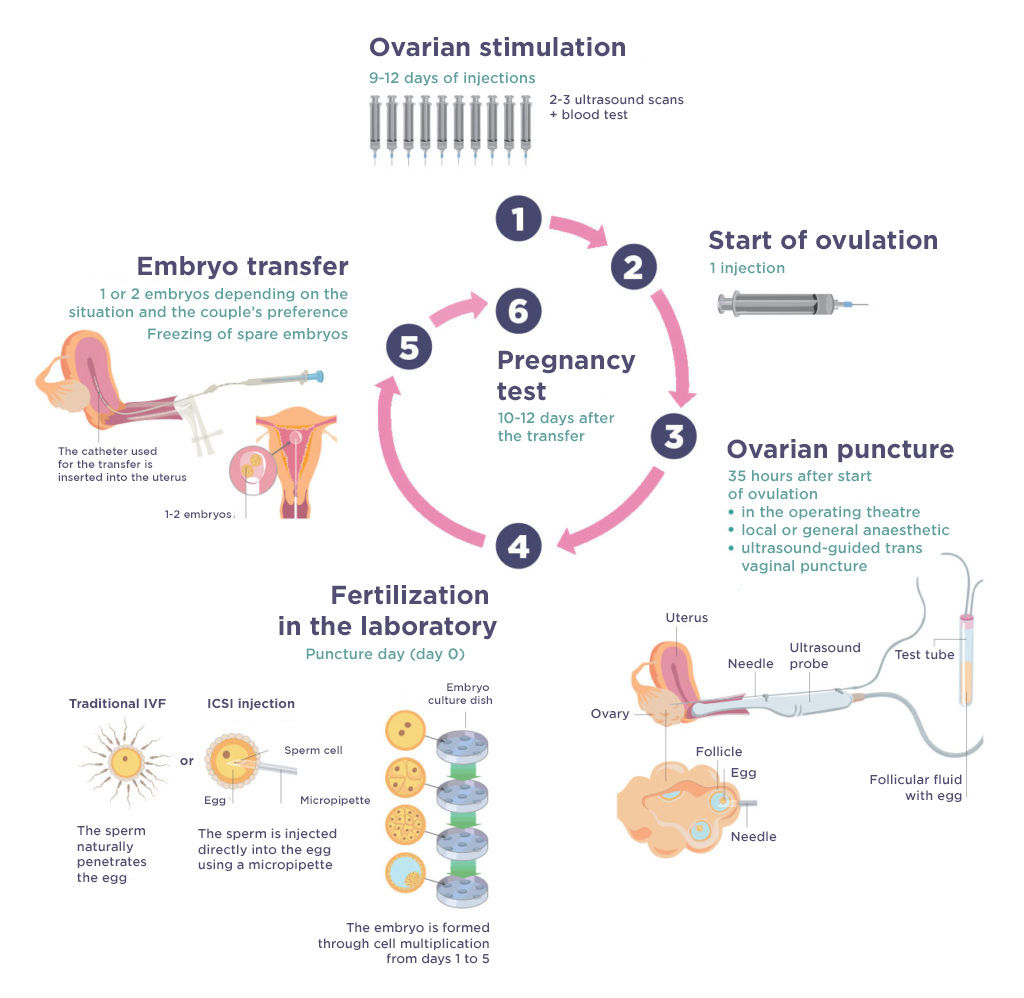
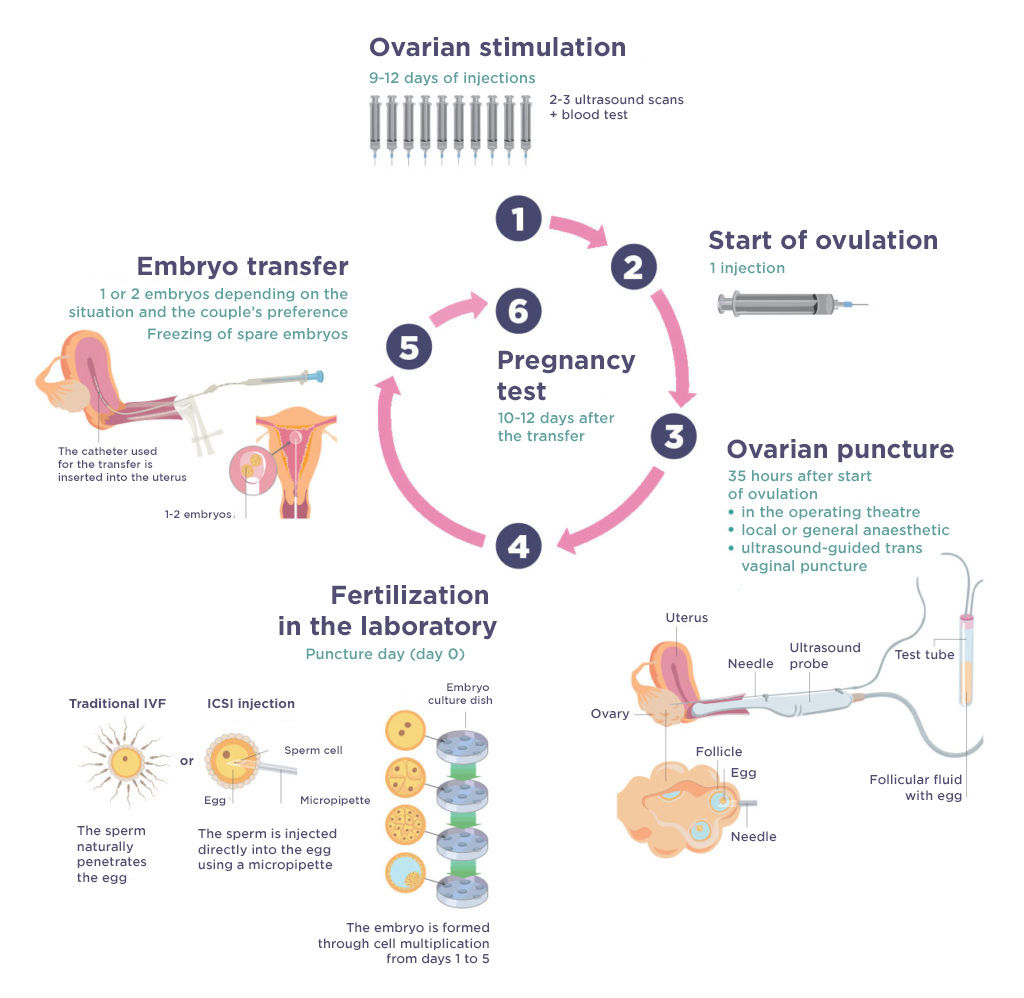
At FertiGenève, the first stage in the IVF process – ovarian stimulation – is performed by REI specialists working in private practice or by the doctors of UMREG, the Reproductive Medicine and Gynaecological Endocrinology Unit at HUG. The patient is given hormone preparations to help her ovaries produce several eggs (oocytes), a process that takes around 10 days. Once the oocytes are ready, based on ultrasound results and hormonal criteria, the woman is given another hormone that enables the oocytes to finish maturing, ready to be fertilized.
This is followed, around 35 hours later, by the egg harvesting process: this second step is performed in an operating theatre (at HUG for UMREG patients, and at Clinique Générale-Beaulieu for patients followed by private practitioners), under a local or general anaesthetic. This is a short procedure performed by gynaecologists, which involves ultrasound-guided transvaginal follicular aspiration.
The tube containing the follicular fluid and the oocytes is then sent to the laboratory in a container at a stable 37°C. The oocytes are placed in an appropriate culture medium and kept in an incubator in conditions close to those found in the fallopian tubes. Sperm collection takes place on the same day. At FertiGenève, the woman’s partner goes directly to the laboratory and produces a sperm sample (through masturbation) in a suitable room.
The next step relies on the embryologists’ expertise. The semen is prepared in order to select the most motile and fertile sperms. Next, in a traditional IVF procedure, several thousand sperms are placed closed to each oocyte in the culture medium. They are all returned to the incubator and fertilization occurs spontaneously.
If sperm quality is poor or spontaneous fertilization is compromised, the embryologists or technicians use a variant of IVF called ICSI (intracytoplasmic sperm injection). This involves selecting a motile sperm cell and injecting it directly into the ovocyte using a micropipette.
The embryos remain in the incubator for five to six days. The embryologists then select those that offer the best chances of a pregnancy. One, or sometimes two, embryos are transferred to the uterus. At FertiGenève, this swift and painless procedure is performed by a gynaecologist in a specially equipped room in the laboratory.
The additional embryos that will not be used immediately are frozen at -196°C, to enable them to be used, if necessary, in a further attempt or to have a second child.
